Jul 14, 2020 | By Tim Stoddart
The Connection Between Childhood Trauma and Substance Use Disorder
Addiction Resources
It’s safe to say there’s a distinct connection between childhood trauma and Substance Use Disorder (SUD). As science and research continue to make advances in the behavioral health and addiction spaces, many still continue to look for answers for addiction. Addiction is complex and stigmatized in popular culture as being weak or unable to have the willingness to change. However, for those who have experienced childhood trauma; these distinct events can follow individuals to adulthood for the long-term, creating maladaptive patterns, mental health and substance abuse issues.
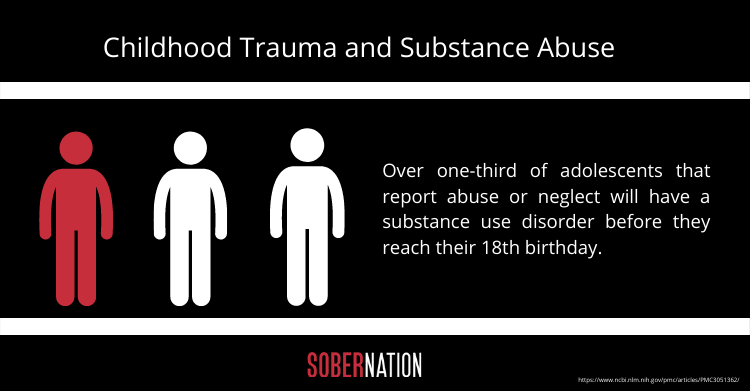
While rates of addiction are high for adult survivors of trauma, these numbers can be even higher for children. Where psychological and emotional development are crucial to the path of adulthood, these factors can be greatly impacted by trauma – ultimately developing unhealthy relationships with substances. For example, according to the National Institute of Health (NIH), more than one third of adolescents that report abuse or neglect will have a substance use disorder before they reach their 18th birthday.
To get a full understanding of the correlation between childhood trauma and substance abuse, we must look at all causes and reactions of trauma, addiction, and the brain affected by these.
Causes of Childhood Trauma
Trauma can most commonly be defined as an individual experiencing a deeply distressing or disturbing event that disrupts the person’s ability to cope, diminishes their sense of self, and ability to experience a full range of emotions. According to a survey conducted by the World Health Organization, a third of the 125,000 people surveyed in 26 different countries noted that they have experienced trauma. Childhood trauma can be more accurately described when a child’s safety feels threatened by an event they’re either involved in or witness. A number of situations or where this can happen can include but not be limited to:
- Physical, sexual, or psychological abuse
- Neglect
- Separation from a parent
- Complex trauma
- Invasive medical procedures
- Substance use disorder in the family
- War experiences
- Life-threatening illness
- Bullying
- Violence
- Natural disasters
- Loss or grief
These type of traumatic experiences can create strong reactions after the incident, creating life-long patterns if not addressed. Even if an adult-figure attempts to keep a child safe, these events can still happen. If a child does happen to be unsafe, the child can feel helpless, terror, and extreme amounts of fear for years to come. The children who are unsafe or lack protection can also become overwhelmed by the extreme stress of emotional and physical responses that follow the traumatic event. These type of emotional, physical, and psychological reactions are commonly referred to as post-traumatic symptoms. Symptoms can vary from person to person, and often are more subjective to the response rather than the trigger.
The Effect of Childhood Trauma on the Brain
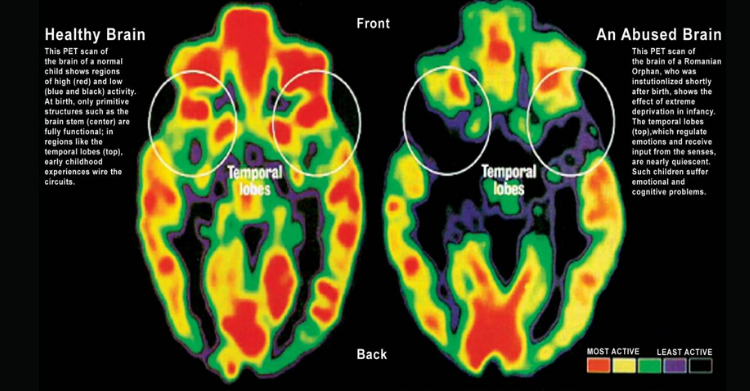
Since the brain is not fully developed until the age of 25, the effect of childhood trauma can severely alter a child’s growth and development. While brains are adaptable, trauma causes physical changes to a child’s brain. The most noticeable changes occur to the Hippocampus which help regulate chemicals such as cortisol – the body’s main stress hormone. This hormone works with different parts of the body to determine mood, motivation, and fear. Cortisol is also known as the “fight or flight” hormone in that it can alter or shut down survival mechanisms that get in the way of functioning.
In addition to the Hippocampus, the cingulum-hippocampus projection (CGH-R) is severely altered. This part of the brain helps emotional regulation and processing information. While not only these two components of the brain are altered, there are more than three other sections of the brain that are physically changed. Stress and abuse can change the shape and connections within the brain, and the prefrontal cortex, which helps determine behavior, cognition, and emotional regulation can also be impacted by trauma. These changes in the brain typically rapidly occur and often effect an impacted child for the rest of their life, no matter if interventions have been implemented.
According to psychiatrist and traumatic stress expert, Bessel van der Kolk, negative childhood experiences can set our brains to constantly feel danger and fear. This can be attributed to the functioning of the amygdala in the brain, often more sensitive to reactions and minor triggers. Over time, fear responses are triggered by less threatening situations than that of a person who hasn’t experienced trauma. In the seen image below, we can see the differences in a normal child’s brain vs a 7-year-old’s brain who has experienced Complex Trauma.
With these altered brain pathways and neuroreceptors are more sensitive to stressful situations, it makes sense that an individual who has experienced childhood trauma needs a source of comfort from these heightened states of fear. Temporarily found in drug and alcohol addiction or process addiction including eating disorders, gambling or sexual addiction, the euphoria these behaviors create involves surges of chemicals and other neurotransmitters in different areas of the brain’s reward circuit.
Just as changes in the brain happen due to trauma, changes in the brain also happen due to substance abuse. The person who has been traumatized can have an insatiable craving for relief or fulfillment and more easily resort to higher risk behaviors than those who haven’t experienced trauma. Drugs, alcohol, and other high risk behaviors can produce large surges of dopamine, reinforcing the need for repeated use of the behavior. Combined with changes in the brain from trauma, the need for larger surges of dopamine teaches the brain to seek out drugs instead of healthier coping mechanisms – ultimately leading to addiction. This quick and fast relief can additionally leave the person vulnerable, creating higher risks for more trauma.
The Manifestation of Childhood Trauma
More often than not, trauma manifests itself in children in a number ways physically, emotionally, and psychologically. Trauma’s effect physically can produce larger amounts than adrenaline and cortisol than the body already creates, activating processes of fight, flight, or freeze. Overtime, these reactions can become re-stimulated in situations that may have triggered memories or associations with the traumatic event but are not necessarily life-threatening.
Psychological reactions of trauma can be attributed to a number of symptoms that can include:
- Exhaustion
- Sadness
- Anxiety
- Numbness
- Dissociation
- Confusion
- Agitation
While these are some of the most common symptoms, many other symptoms can be seen survivors of a traumatic incident, however are not necessary to have been affected by trauma.
Psychological Effects of Childhood Trauma in Adulthood
As children, the struggle to keep these memories and reactions at bay can be exhausting. Victims of trauma can feel vulnerable. To make sense of what happened, individuals often develop new belief systems and internal maps to help cope. Taking these emotional wounds into adulthood, individuals can create negative belief systems or perceptions of a false identity in order to protect themselves and feel safe and accepted. It’s common for individuals who have experienced childhood trauma to bury feelings and walk through the world with unmet needs. Most fear if they show their true selves, they’ll be abandoned, rejected, and unloved. These unmet needs can also result in substance abuse.
Another psychological pattern childhood trauma can carry to adulthood is negative self-talk. Victimized as children, adults can keep themselves in a victim mentality driving the loop of disempowerment and making an individual believe they have no control over their lives. As children, an individual may not have control of their environment or situation, however, individuals don’t have to remain victim for the rest of their lives. It can be a difficult pattern to break, but not impossible with therapy and counseling.
In addition, if a child has grown up in a household where there is an unhealthy expression of anger, the child may begin to believe that showing anger isn’t appropriate. If the traumatic incident an individual experienced had to do with violence or anger, the child may begin to suppress anger and believe it to be a violent emotion. Carrying into adulthood, individuals may suppress feelings, and be unable to express anger. In this situation it’s important to remember that anger is a normal emotion that we all experience. For those that have experienced this type of trauma may carry anger with them but lack the capacity to express it straightforwardly, ultimately expressing it through passive-aggressiveness.
If the type of trauma someone experienced as a child was neglect or abandonment, one may have picked up coping skills such as burying their anger, fear, and frustrations in order to not be neglected again. Though not outwardly recognizing this, all of the previous mentioned coping mechanisms are picked up slowly overtime and can result in a quicker path to substance abuse to make up for these unmet needs and unspoken feelings.
Trauma-Informed Addiction Treatment
It’s clear to note that childhood trauma and substance abuse should be addressed simultaneously as a co-occurring issue in an addiction treatment and trauma-informed care setting. Trauma informed addiction treatment is a definitive approach on the basis of how trauma affects the brain and uses this information to dictate clinical practices and addresses symptoms of trauma. These approaches are not necessarily formulated to address and process the actual event, but the symptoms that are associated with it.
While there are a number approaches to trauma-informed addiction treatment, there are three main points included in treatment trauma in this element which include:
- To promote an understanding of symptoms from a strength based approach
- Minimize the risk of re-traumatizing the patient
- Offer and identify supports that are trauma informed.
Trauma-informed addiction treatment additionally runs on the basis of the autonomic nervous system that responds to trauma. Comprised of the sympathetic and parasympathetic nervous system, the sympathetic nervous system increases stimulation including an increase in heart rate, while the parasympathetic nervous system relaxes the individual lowering heart rate. While facilities vary, a number of modalities in trauma-informed treatment offers services to help reduce the overstimulated sympathetic nervous system by increasing activation of the parasympathetic nervous system.
These modalities can include but not be limited to the following:
- Individual therapy
- Peer Support Groups
- Mindfulness, yoga, meditation and relaxation techniques
- Dialectical behavioral therapy including emotional regulation and distress tolerance skills
- Desensitization therapy
- Pharmacotherapy
Helping to address these root issues with trauma-informed care can create a better chance in helping individuals create long-term sobriety. Individuals who have experienced childhood trauma and use drugs and alcohol as a way handle internal turmoil associated with these incidents use to find relief and not necessarily because it’s a fun way to navigate life.
If you or a loved one are struggling with childhood trauma and substance abuse, we’re here to help you live the live you deserve. Call Sober Nation’s toll-free hotline at 866-317-7050 or find a treatment center in your area, here.
